*Please note: This slide show represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
Establishing and maintaining remission of disease symptoms prior to and during pregnancy are essential, and a variety of medications are available to achieve this goal.
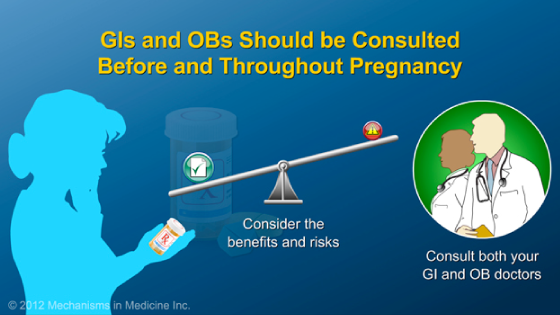
The benefits of treatment and making sure the disease remains inactive during pregnancy far outweigh the concerns associated with the risk of these therapies.
The same medication classes we use in non-pregnant women are available for treating disease while pregnant. These include: aminosalicylates, corticosteroids, immunomodulators, and anti-TNF therapies.
The aminosalicylates are anti-inflammatory drugs used to treat mild to moderate cases of IBD. They impede the ability of the body to make chemical signals, known as cytokines, that promote inflammation. Examples include mesalamine and sulfasalazine. It is important if you are taking sulfasalazine that you take extra folic acid daily (2 mg per day).
These agents can be used to curb the inflammation present in ulcerative colitis and in mild cases of Crohn’s disease. This class of medication is considered a safe choice in pregnancy because aminosalicylates have few or minimal side effects.
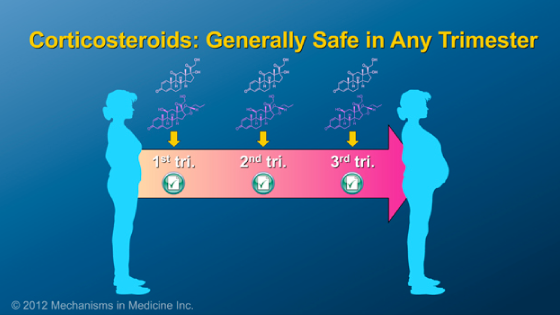
Corticosteroids are powerful and fast-acting anti-inflammatory drugs. Examples of corticosteroids used in the treatment of IBD, include prednisone and budesonide.
Corticosteroids are generally safe to use in any trimester.
Please be sure to talk to your obstetrician and gastroenterologist about the implications of using corticosteroids and what precautions, if any, you should take.
Immunomodulators such as azathioprine and 6-mercaptopurine suppress the immune system, but unlike corticosteroids, are given for longer periods of time to maintain a steroid-free remission. It is best to be on a stable dose of this medication prior to getting pregnant. It is important to not stop these medications without checking with your gastroenterologist.
Anti-TNF therapies (infliximab, adalimumab, and certolizumab pegol) are also used to treat IBD before and during pregnancy when other drug options have proven ineffective.
These medications decrease inflammation and maintain a state of remission by blocking the cytokine, tumor necrosis factor-alpha (TNF-α), which is a major chemical signal involved in the inflammation process.
These medications are safe to use during pregnancy and are often the reason patients feel well enough to consider getting pregnant. The timing of when patients receive their infusions or injections during pregnancy needs to be discussed with your gastroenterologist.
It is also important to talk to your gastroenterologist and pediatrician about the timing of vaccines for your newborn baby if you received anti-TNF therapies during pregnancy. Live vaccines such as the Rotavirus vaccine should not be given to your baby in the first 6 months of your baby’s life if you received these medicines in during your pregnancy. All other vaccines should be given to your baby as scheduled as they are not live.
Methotrexate and thalidomide are two drugs that MUST be avoided in pregnant women because these medications can lead to birth defects and miscarriages. Women who are taking either of these drugs to treat their IBD MUST discuss other treatment options with their doctor long before conceiving.
With the exception of methotrexate and thalidomide, all medications we use to treat your IBD before pregnancy can be safely used during pregnancy.
It is important to check with your gastroenterologist before stopping ANY medications. Your obstetrician may want you to stop some of these therapies but it is best that your gastroenterologist call your obstetrician to discuss as to why you should stay on these medications.
As with all medications, there are risks of varying severity associated with each of the classes of drugs used to treat IBD.
Pregnant women who are considering taking any of these medications are strongly encouraged to consult both their obstetrician and gastroenterologist prior to and throughout their pregnancy in order to determine the most suitable course of treatment.
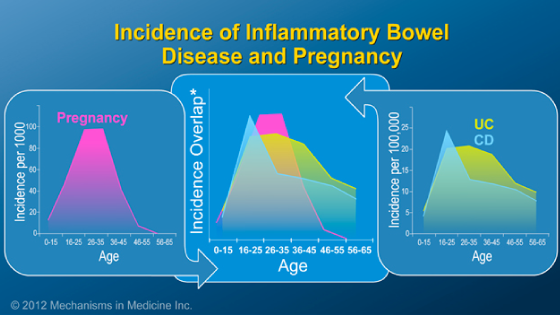
This slide show describes treatment options during pregnancy for women with inflammatory bowel disease (IBD).
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about IBD which will help other patients, caregivers and families.